Converge I can tell you about pain delves into the multifaceted nature of pain, exploring its diverse forms, underlying mechanisms, and the profound impact it has on individuals. We’ll uncover the intricate interplay of physical, emotional, and social factors that converge to shape the pain experience, examining how lifestyle choices, communication strategies, and various pain management techniques can make a real difference.
From understanding the biology of pain to navigating the emotional toll, this comprehensive exploration aims to empower readers with knowledge and resources to better understand and manage their own pain, or the pain of those around them.
This journey through pain’s complexities begins by examining the fundamental types of pain, from acute to chronic and neuropathic, and the intricate biological processes that underpin our perception of discomfort. We’ll explore the significant role of psychological and emotional factors in influencing pain experience, drawing comparisons across different populations to illustrate the multifaceted nature of this human condition. Tables will visually represent crucial insights, including pain triggers, symptoms, and potential causes.
This groundwork will provide a strong foundation for understanding the convergence of various factors that contribute to an individual’s pain experience.
Understanding Pain
Pain is a complex and multifaceted human experience, deeply interwoven with our physical, psychological, and social well-being. It serves as a vital warning signal, alerting us to potential harm and prompting us to take corrective action. However, understanding the nuances of pain goes beyond simple discomfort; it encompasses a spectrum of sensations, influenced by a multitude of factors.
This exploration delves into the various types of pain, the biological processes involved, the psychological dimensions, and the differing experiences across diverse populations.
Types of Pain
Pain can be broadly categorized into acute and chronic pain, each with its own characteristics and implications. Acute pain is a short-term, often sharp, sensation that typically arises in response to tissue damage, injury, or inflammation. Chronic pain, conversely, persists for an extended period, often exceeding three months, and can significantly impact daily life. It may not always be directly linked to an easily identifiable injury.
Converge’s “I Can Tell You About Pain” is a powerful album, really hitting you with its raw emotion. Speaking of raw emotion, I was thrilled to hear about The Smiths’ deluxe reissue of “The Queen is Dead” the smiths announce deluxe reissue of the queen is dead. It’s a great reminder of the band’s influence, and honestly, their pain-filled tunes often evoke similar feelings to Converge’s more intense moments.
Hopefully, the new reissue will inspire a fresh wave of appreciation for the band’s dark and brilliant soundscapes, just like Converge’s music inspires me.
Neuropathic pain, a distinct type, results from damage or dysfunction in the nerves themselves, often manifesting as shooting, burning, or tingling sensations.
Biological Mechanisms of Pain Perception
Pain perception is a complex process involving specialized receptors, nerve pathways, and the central nervous system. Nociceptors, sensory nerve endings, detect potentially harmful stimuli, translating them into electrical signals. These signals travel along specific pathways to the spinal cord and then ascend to the brain. The brain interprets these signals, assigning meaning to the sensation as pain. The intensity and quality of the pain experience are influenced by various factors along this pathway, including the type of stimulus, the individual’s pain sensitivity, and the presence of other conditions.
Psychological and Emotional Factors in Pain
Psychological and emotional factors play a significant role in how individuals experience pain. Stress, anxiety, depression, and past trauma can all amplify pain perception or even create pain where no physical injury exists. Conversely, positive emotions and coping mechanisms can mitigate the pain experience. These psychological factors can be as impactful as the physical source of pain, highlighting the intricate interplay between mind and body in pain management.
Pain Experience Across Populations
The pain experience can vary significantly across different populations, influenced by age, gender, cultural background, and other socio-economic factors. For instance, older adults may experience different pain thresholds and types of pain compared to younger adults. Cultural backgrounds can shape perceptions of pain and influence how individuals express and manage their pain. Gender differences in pain perception are also recognized, though the exact mechanisms are still being investigated.
These factors underscore the importance of personalized approaches to pain management.
Pain Triggers and Associated Responses, Converge i can tell you about pain
| Trigger | Pain Type | Symptoms | Potential Causes |
|---|---|---|---|
| Sprained ankle | Acute pain | Sharp, localized pain; swelling, bruising | Sudden twisting or impact to the ankle joint |
| Chronic back pain | Chronic pain | Dull, aching pain in the back; stiffness, limited mobility | Muscle strain, degenerative disc disease, arthritis |
| Burning sensation in the feet | Neuropathic pain | Intense burning, tingling, numbness | Diabetes, nerve compression, multiple sclerosis |
| Dental procedure | Acute pain | Sharp, localized pain in the mouth | Stimulation of dental nerve endings |
Pain is a complex interaction between physical stimuli, psychological factors, and individual experiences. Understanding these different aspects is crucial in developing effective pain management strategies tailored to the specific needs of each individual.
Converging Factors in Pain
Pain is a complex experience, significantly influenced by a multitude of interacting factors. Understanding these converging forces is crucial for effective pain management, as addressing one aspect may not be sufficient. It’s often a combination of physical, emotional, and social elements that contribute to the overall pain experience, making a holistic approach essential.The experience of pain is not simply a response to tissue damage.
Psychological and social factors play a critical role in shaping how individuals perceive and react to pain. Stress, anxiety, and depression can amplify the sensation of pain, while support systems and coping mechanisms can lessen its impact. This multifaceted nature underscores the importance of considering all contributing elements when developing pain management strategies.
Physical Factors Contributing to Pain
Physical factors, such as tissue damage, inflammation, and nerve dysfunction, are fundamental to pain perception. Injuries, illnesses, and chronic conditions can all trigger or exacerbate pain. The severity and duration of pain often correlate with the extent of physical damage or dysfunction. For instance, a sprained ankle may result in acute pain that subsides over time, while a chronic condition like arthritis can cause persistent and debilitating pain.
Emotional Factors Influencing Pain
Emotional factors, including stress, anxiety, and depression, can significantly influence pain perception. Stress hormones can increase pain sensitivity, making individuals more susceptible to pain signals. Conversely, positive emotions and a strong sense of well-being can contribute to a more resilient response to pain. For example, individuals experiencing high levels of stress may report increased pain intensity compared to those with lower stress levels.
Social Factors in Pain Perception
Social factors, such as support systems and cultural norms, also play a role in how individuals experience and manage pain. Strong social support networks can buffer the negative impact of pain, providing emotional comfort and practical assistance. Cultural norms and beliefs can influence pain expression and treatment preferences. For example, in some cultures, open displays of pain are encouraged, while others may discourage emotional expression, potentially impacting pain management strategies.
Pain Patterns and Underlying Causes
Different pain patterns can arise from various underlying causes. Acute pain, often associated with injuries or sudden events, typically has a clear cause and limited duration. Chronic pain, on the other hand, persists for extended periods, sometimes with unclear or multiple contributing factors. Fibromyalgia, for example, is a chronic pain syndrome with a complex interplay of physical, emotional, and social factors, making pain management challenging.
Lifestyle Choices and Pain Management
Lifestyle choices significantly impact pain management. Diet, exercise, and stress management techniques can all influence pain levels. A balanced diet, regular exercise, and effective stress management strategies can contribute to a healthier response to pain. Conversely, unhealthy lifestyle choices can worsen pain and complicate recovery.
Impact of Lifestyle Factors on Pain Levels
| Lifestyle Factor | Positive Impact | Negative Impact |
|---|---|---|
| Balanced Diet | Provides essential nutrients for tissue repair and reduces inflammation. | Poor nutrition can lead to deficiencies, weakening the body’s ability to heal and potentially increasing pain. |
| Regular Exercise | Strengthens muscles, improves flexibility, and reduces stress. | Lack of exercise can lead to muscle weakness, poor posture, and increased vulnerability to injury. |
| Effective Stress Management | Reduces stress hormones that increase pain sensitivity. | Chronic stress can exacerbate pain and hinder recovery. |
| Adequate Sleep | Allows the body to repair and regenerate, promoting healing. | Sleep deprivation can increase pain sensitivity and hinder the body’s natural pain-relieving mechanisms. |
| Social Support | Provides emotional comfort and practical assistance, reducing stress and promoting coping mechanisms. | Lack of social support can increase isolation and stress, potentially worsening pain. |
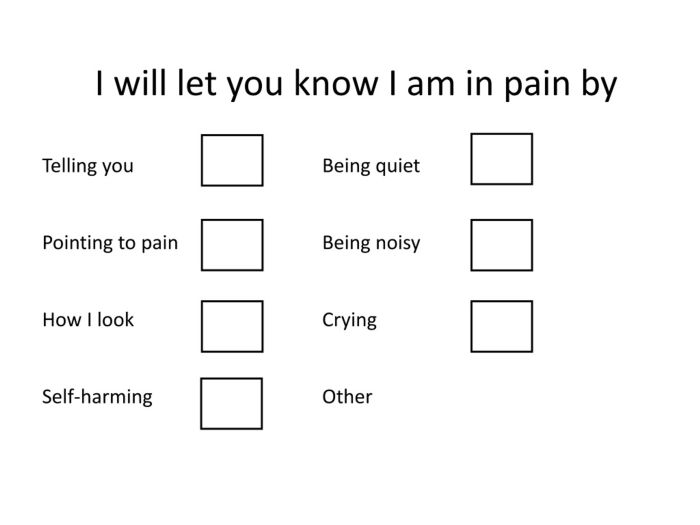
Communicating about Pain
Effective communication about pain is crucial for successful pain management. It’s a two-way street where both patients and healthcare providers play vital roles in understanding and addressing the experience. Without clear and honest communication, the path to relief can be significantly hindered. This crucial aspect often gets overlooked, yet it’s fundamental to effective treatment plans.Open and honest communication between patients and healthcare professionals is paramount.
Patients must feel comfortable expressing their pain experience, while healthcare providers need to actively listen and ask clarifying questions. This collaborative effort creates a shared understanding of the pain, which is essential for developing an appropriate treatment strategy. This shared understanding is vital for identifying the underlying cause of the pain and creating a tailored management plan.
Effective Communication Strategies for Individuals Experiencing Pain
Patients can significantly improve their pain communication by actively describing their pain. This involves using specific descriptors, including location, intensity, quality (e.g., sharp, dull, throbbing), duration, and any associated symptoms. Furthermore, they should note any triggers or factors that seem to exacerbate or alleviate the pain. It’s important to avoid vague language and instead provide concrete details that healthcare providers can use to accurately assess the situation.
Importance of Open and Honest Communication
Open and honest communication between patients and healthcare providers is essential for effective pain management. Patients must feel empowered to express their concerns and experiences without fear of judgment or dismissal. Healthcare providers, in turn, must actively listen and respond empathetically to the patient’s perspective. This reciprocal exchange fosters trust and facilitates a collaborative approach to pain management.
Examples of Questions Patients Can Ask
Patients can ask a range of questions to gain a deeper understanding of their pain. Examples include: “What are the potential causes of my pain?”, “What are the different treatment options available?”, “What are the potential side effects of the treatments?”, “What is the expected recovery time?”, “How can I manage my pain at home?”. These questions demonstrate a proactive approach to understanding their condition and enable informed decisions about their care.
Comparison of Pain Communication Methods
| Method | Strengths | Weaknesses |
|---|---|---|
| Verbal Description | Allows for detailed explanation of pain characteristics, including location, intensity, and quality. It enables the patient to express the subjective experience of pain. | Can be subjective and influenced by individual perception. May be difficult for patients to articulate complex pain experiences. Can be time-consuming. |
| Visual Analog Scale (VAS) | Provides a standardized, objective way to measure pain intensity. Easy to understand and use. | Doesn’t capture the complexity of pain beyond intensity. May not be suitable for all patients, especially those with cognitive impairments. |
| Pain Diaries | Allows for tracking pain patterns over time, identifying triggers, and monitoring treatment effectiveness. | Requires consistent effort from the patient. May not be suitable for patients with memory problems or limited literacy. Can be cumbersome to maintain. |
Tips for Improving Pain Communication
- Use specific and descriptive language when describing pain.
- Keep a pain diary to track pain patterns and triggers.
- Bring a list of questions to the appointment.
- Ask for clarification on any medical terms or procedures.
- Actively listen to the healthcare provider’s responses and ask follow-up questions.
- Share past experiences with pain and any previous treatments.
- Document any pain relief strategies that have worked in the past.
Pain Management Strategies
Understanding pain is a crucial first step, but effective pain management requires a multifaceted approach. This involves exploring various strategies, considering individual needs, and acknowledging the limitations of different techniques. Personal experiences and professional guidance are vital in finding the most suitable methods for managing pain effectively.Effective pain management is not a one-size-fits-all solution. A personalized strategy often involves a combination of approaches, tailored to the specific type, intensity, and location of the pain.
This approach acknowledges the diverse nature of pain experiences and the importance of individual responses to different treatments.
Medication
Pain medications are a cornerstone of pain management, providing relief by altering the body’s response to pain signals. Different types of medication target various aspects of the pain pathway, offering varying degrees of efficacy and potential side effects. Careful consideration of the specific medication, dosage, and potential interactions is essential.
Physical Therapy
Physical therapy plays a vital role in pain management, particularly for musculoskeletal issues. This approach involves exercises, manual therapy techniques, and other interventions aimed at improving function, reducing pain, and restoring mobility. Physical therapy can be extremely beneficial in rehabilitating injuries and promoting long-term pain management strategies.
Alternative Therapies
Alternative therapies, such as acupuncture, massage therapy, and mindfulness techniques, offer complementary approaches to pain management. These therapies aim to address the root causes of pain, promote relaxation, and reduce stress, often working in conjunction with other pain management strategies.
Effectiveness and Limitations of Different Approaches
The effectiveness of any pain management strategy varies significantly depending on the individual and the nature of the pain. Factors like the cause of the pain, the individual’s overall health, and their response to the treatment all play a significant role. Limitations exist in all approaches, and understanding these limitations is critical to developing a holistic pain management plan.
Pain Management Resources
- Books: “Chronic Pain Relief” by Dr. X and “Managing Your Pain” by Y are excellent resources for understanding chronic pain and managing it effectively.
- Websites: The National Institutes of Health (NIH) website offers a wealth of information on pain management, as well as resources from reputable pain management organizations.
- Organizations: The American Pain Society and the Arthritis Foundation provide support and resources for individuals experiencing pain.
Comparison of Pain Medications
| Medication | Efficacy | Potential Side Effects |
|---|---|---|
| Acetaminophen (Tylenol) | Generally effective for mild to moderate pain; often a first-line treatment | Liver damage with high doses or prolonged use; may cause allergic reactions in some individuals. |
| Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil) | Effective for various types of pain, including inflammation-related pain. | Gastrointestinal issues (stomach ulcers, bleeding), kidney problems, and allergic reactions. |
| Opioids | Highly effective for severe pain but carries significant risk. | Addiction, respiratory depression, constipation, and nausea. |
Heat Therapy
Heat therapy involves applying heat to the affected area, promoting blood flow and reducing muscle tension. This can be achieved through hot packs, heating pads, or warm baths. Applying heat can be beneficial for reducing pain and stiffness, and in some cases, it can even help to accelerate healing. Always ensure the heat source is not too hot to avoid burns.
Case Studies and Examples
Unveiling the diverse tapestry of pain management requires delving into real-life experiences. This section offers case studies illustrating effective strategies, highlighting both successes and challenges encountered by individuals navigating the complexities of pain. We’ll explore specific types of pain, examining symptom profiles, treatment approaches, and ultimately, outcomes. By understanding these individual journeys, we gain valuable insights into personalized pain management.Understanding how individuals cope with and manage pain is critical to developing comprehensive support systems and treatment plans.
Converge, I can tell you about pain, a raw, visceral feeling. It’s something I’ve been wrestling with lately, and honestly, it’s been a real downer. Speaking of downers, have you seen Noel Gallagher play “Holy Mountain” on Kimmel? It’s a total blast! You can check it out here: watch noel gallagher play holy mountain on kimmel.
The sheer energy and passion in his performance, though, kind of made me realize that even in the face of pain, there’s always room for a bit of joy, a bit of a musical escape. Converge, I can tell you about pain, but I can also tell you about finding a way to dance through it, even if it’s just with a little bit of rock ‘n’ roll.
Each case study provides a glimpse into the human experience of living with chronic pain, offering inspiration and guidance for those seeking effective solutions.
Back Pain Case Study: Sarah’s Journey
Sarah, a 45-year-old office worker, experienced chronic lower back pain for over two years. Initial symptoms included stiffness, radiating pain down her legs, and debilitating muscle spasms. She tried over-the-counter pain relievers, physical therapy, and even a brief stint with opioid medication. Unfortunately, these approaches offered only temporary relief. Sarah’s pain significantly impacted her ability to work and participate in social activities.
She felt isolated and frustrated.Through a multidisciplinary approach, Sarah found success. A combination of targeted exercises, mindfulness techniques, and a dietary adjustment proved beneficial. Regular yoga sessions helped improve flexibility and core strength. Mindfulness practices allowed her to manage stress, a significant contributor to her pain. Furthermore, dietary changes focusing on anti-inflammatory foods led to noticeable improvements in her overall well-being and pain levels.
After six months, Sarah reported a significant reduction in pain intensity and a marked improvement in her quality of life. Her experience demonstrates the potential of holistic approaches to chronic back pain management.
Headache Case Study: David’s Experience
David, a 32-year-old software engineer, suffered from frequent tension headaches. These headaches were characterized by a dull, throbbing pain across his forehead and temples, often accompanied by nausea and sensitivity to light and sound. Initially, David relied on over-the-counter pain relievers, but these provided only temporary relief. He sought professional help when the headaches began impacting his work performance.His journey to effective headache management involved exploring the root causes.
Converge, I can tell you about pain, especially the kind that comes from watching a sibling struggle. It’s a familiar feeling, a kind of shared hurt, isn’t it? Learning to navigate those tricky situations, like understanding and supporting younger siblings, takes a lot of patience and empathy. For more insights on how to provide effective care for younger siblings, check out this helpful guide: Care for Younger Siblings.
Ultimately, though, that shared pain, that empathy, that understanding – it’s all part of the convergence of experience, and it’s something we can all learn from.
A thorough evaluation by a neurologist revealed a link between David’s headaches and stress related to his demanding job. Stress reduction techniques, including meditation and progressive muscle relaxation, became integral components of his treatment plan. Cognitive behavioral therapy (CBT) helped him develop coping mechanisms for stress management. Furthermore, dietary modifications, including reducing caffeine and alcohol intake, also contributed to the reduction of his headache frequency.
Over time, David successfully reduced the frequency and intensity of his headaches, enabling him to lead a more productive and fulfilling life.
Short Descriptions of Pain Management Stories
- Maria, a 60-year-old with osteoarthritis, found relief through a combination of aquatic therapy and a specialized exercise program. This approach improved her mobility and reduced joint pain.
- John, a 28-year-old with fibromyalgia, discovered that incorporating mindfulness practices into his daily routine significantly lessened the severity of his symptoms and enhanced his overall emotional well-being.
- Emily, a 35-year-old with neuropathic pain, found that acupuncture sessions and a supportive community of fellow sufferers provided both physical and emotional support.
Exploring the Impact of Pain
Chronic pain is more than just a physical sensation; it profoundly impacts every facet of a person’s life. It’s a complex experience that affects not only physical well-being but also emotional state, social interactions, and overall quality of life. Understanding these multifaceted consequences is crucial for developing effective pain management strategies and support systems.The relentless nature of chronic pain can lead to a cascade of challenges, often exceeding the immediate discomfort.
Individuals struggling with persistent pain may experience significant limitations in their daily activities, relationships, and professional lives. This impact can range from subtle adjustments to profound alterations in lifestyle. This exploration will delve into the far-reaching effects of pain, examining the personal and societal costs associated with this pervasive condition.
Physical Impact of Chronic Pain
Chronic pain often manifests as persistent aches, stiffness, or tenderness, limiting movement and causing fatigue. This physical impact can range from simple discomfort to debilitating conditions, significantly reducing functional capacity. Examples include difficulty performing basic tasks like dressing, bathing, or walking. Individuals may experience muscle weakness, joint stiffness, and decreased range of motion. The pain itself can trigger a cascade of physiological responses, further impacting physical well-being.
Emotional Toll of Chronic Pain
Chronic pain can significantly impact mental health. The constant discomfort and uncertainty about the future can lead to anxiety, depression, and feelings of hopelessness. The emotional distress associated with pain can manifest as irritability, frustration, and difficulty concentrating. These emotional challenges often complicate pain management and contribute to a lower quality of life. Moreover, societal expectations and perceived limitations can add further emotional strain on individuals.
Social and Relationship Impact
Chronic pain can strain social relationships and create difficulties in maintaining social activities. The limitations imposed by pain may lead to social isolation, as individuals find it challenging to participate in social events or maintain close relationships. The emotional burden of pain can also negatively affect communication and intimacy within relationships. For instance, a person with chronic back pain might find it difficult to engage in physical activities with their partner, impacting their intimacy and emotional connection.
Economic Costs of Pain
The economic burden of chronic pain is substantial. Direct costs include healthcare expenses, such as medication, therapy, and medical procedures. Indirect costs encompass lost productivity due to missed work, reduced work capacity, and increased absenteeism. The financial strain on individuals and families can be significant, impacting their ability to maintain their standard of living. Furthermore, the long-term impact of chronic pain on employment prospects and earnings potential is a major consideration.
Impact on Daily Activities
Chronic pain can severely restrict individuals’ ability to perform daily tasks. Simple activities like household chores, personal care, and even socializing can become arduous or impossible. For instance, someone with chronic neck pain might find it difficult to read, work on a computer, or even participate in casual conversations. The constant need for rest and the avoidance of activities can create a vicious cycle, impacting overall well-being.
Support Resources for Pain Management
Numerous resources are available to support individuals dealing with chronic pain. These include:
- Pain management clinics: These specialized clinics offer comprehensive care, including physical therapy, medication management, and psychological support.
- Support groups: Connecting with others who understand the challenges of chronic pain can provide emotional support and practical advice.
- Self-help resources: Books, websites, and online communities offer valuable information and coping strategies for managing pain.
- Physical therapists: Therapists can develop tailored exercise programs to improve strength, flexibility, and pain management techniques.
Epilogue: Converge I Can Tell You About Pain
In conclusion, converge I can tell you about pain offers a holistic perspective on this universal human experience. By understanding the multifaceted nature of pain, from its biological underpinnings to its impact on daily life, we can better equip ourselves and others to navigate the challenges it presents. The interplay of physical, emotional, and social factors, combined with effective communication and targeted management strategies, provides a pathway towards mitigating the suffering associated with pain.
This exploration underscores the importance of compassionate understanding and proactive approaches to pain management, empowering individuals to reclaim control and well-being.