Reverse Dental Bone Loss: This fascinating, yet often overlooked, dental issue presents a unique challenge to both patients and dentists. It involves a surprising decline in jawbone density, sometimes due to seemingly innocuous factors. This comprehensive guide delves into the intricacies of this condition, exploring its causes, diagnosis, treatment, and prevention strategies.
Understanding the complexities of reverse dental bone loss requires examining various aspects. From the initial definition and pathophysiology to the diverse treatment options and preventive measures, this exploration aims to equip readers with the knowledge to better understand this often-misunderstood condition.
Defining Reverse Dental Bone Loss
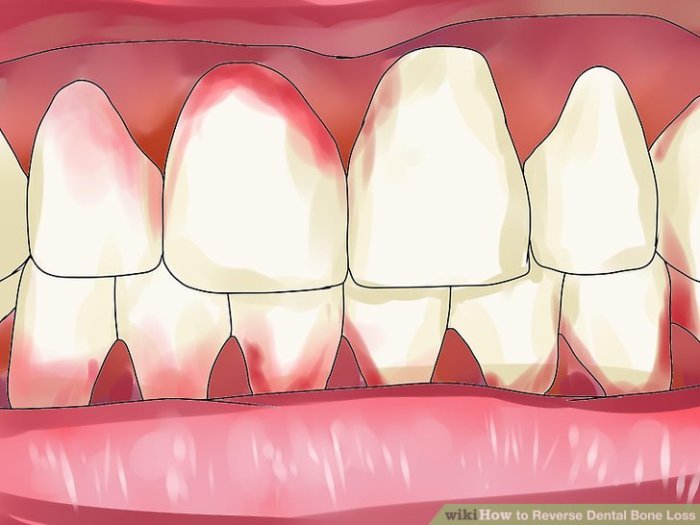
Reverse dental bone loss, often referred to as alveolar bone loss, is a critical issue in dentistry that describes the progressive resorption of the alveolar bone surrounding the teeth. Unlike the more common scenario of bone loss due to periodontal disease, reverse bone loss presents a unique set of challenges in diagnosis and treatment. This condition is characterized by a reduction in bone density and structure, impacting the overall stability and support of the teeth.Understanding the intricacies of reverse dental bone loss requires a multifaceted approach, encompassing its pathophysiology, stages, classifications (if any), and contributing factors.
A comprehensive understanding is crucial for developing effective strategies to mitigate its detrimental effects on oral health.
Defining Reverse Dental Bone Loss
Reverse dental bone loss, in contrast to typical periodontal bone loss, involves a decrease in the alveolar bone height around teeth, rather than a loss of bone support. This reduction in bone density can lead to tooth mobility and instability. The exact mechanisms behind reverse bone loss are not fully elucidated but are believed to involve a complex interplay of genetic predisposition, systemic diseases, and local factors like occlusal forces and inflammation.
It’s important to note that reverse bone loss is not simply the opposite of typical bone loss; the underlying mechanisms and risk factors are distinct.
Pathophysiology of Reverse Dental Bone Loss
The pathophysiology of reverse dental bone loss is complex and not fully understood. However, several contributing factors and mechanisms are suspected to play a role. These factors include systemic conditions, such as hormonal imbalances or metabolic disorders, and local factors, like occlusal forces and inflammation. Genetic predisposition may also contribute to the development of reverse bone loss. The exact interplay of these factors is still being investigated.
Stages of Reverse Dental Bone Loss
The progression of reverse dental bone loss can be broadly categorized into stages, although precise definitions and boundaries may vary depending on the specific case and the evaluation method. Early stages often involve subtle changes in bone density, while later stages may result in significant bone resorption and potential tooth mobility. Detailed clinical and radiographic assessments are crucial to monitor the progression and tailor treatment accordingly.
The stages are not rigidly defined, and the progression can vary greatly between individuals.
Classifications of Reverse Dental Bone Loss
Currently, there is no standardized classification system specifically for reverse dental bone loss. Different diagnostic criteria and evaluation methods may be used depending on the clinician and the specific case. Research efforts are ongoing to develop a more comprehensive and standardized classification system to facilitate better understanding and treatment planning.
Factors Contributing to Reverse Dental Bone Loss
Understanding the contributing factors to reverse dental bone loss is crucial for developing effective preventive strategies. This table provides an overview of potential factors, their descriptions, potential impacts, and preventative measures.
| Factor | Description | Potential Impact | Prevention Strategies |
|---|---|---|---|
| Systemic Diseases (e.g., Diabetes, Hypothyroidism) | Underlying medical conditions can affect bone metabolism and increase the risk of bone loss. | Can exacerbate bone resorption and decrease bone density, potentially accelerating reverse bone loss. | Manage and control systemic diseases through appropriate medical interventions. |
| Hormonal Imbalances | Fluctuations in hormones, such as estrogen or testosterone, can impact bone density. | Hormonal imbalances can disrupt bone remodeling processes, leading to bone loss. | Address hormonal imbalances with appropriate medical guidance. |
| Local Factors (e.g., Occlusal Forces, Trauma) | Forces applied to the teeth or surrounding tissues can contribute to bone resorption. | Excessive or misaligned occlusal forces can induce stress on the alveolar bone, leading to bone loss. | Ensure proper alignment and occlusal equilibrium through orthodontic or restorative procedures. |
| Genetic Predisposition | Certain genetic factors may increase the likelihood of experiencing reverse bone loss. | Inherited traits can influence bone density and structure, making some individuals more susceptible to bone loss. | Regular dental check-ups for early detection and potential intervention. |
Causes and Risk Factors
Reverse dental bone loss, a disheartening process that weakens the jawbone structure supporting teeth, stems from a complex interplay of intrinsic and extrinsic factors. Understanding these factors is crucial for effective prevention and treatment strategies. This often overlooked issue can lead to significant oral health problems, impacting not only the aesthetics but also the overall functionality of the mouth.Identifying the specific causes allows for targeted interventions, enabling individuals to proactively manage their risk and maintain optimal oral health.
This understanding is vital to mitigating the progression of bone loss and preserving the integrity of the jaw.
Intrinsic Factors
Intrinsic factors are internal predispositions that increase susceptibility to reverse dental bone loss. These factors are often deeply rooted in genetics, age-related physiological changes, and systemic health conditions. Genetic predispositions to lower bone density and systemic illnesses can significantly impact the jawbone’s ability to maintain its structure.
- Genetics: Inherited traits play a significant role in determining bone density and metabolism. Individuals with a family history of osteoporosis or low bone mineral density are more likely to experience reverse dental bone loss.
- Age: As we age, our bodies undergo natural changes, including a decline in bone turnover. This decreased bone turnover can contribute to a reduction in bone mass and increased susceptibility to bone loss.
- Systemic Diseases: Certain systemic conditions, such as osteoporosis, rheumatoid arthritis, and diabetes, can impact bone health and increase the risk of reverse dental bone loss. These conditions can interfere with normal bone remodeling processes, leading to a reduced ability to maintain bone density.
Extrinsic Factors
Extrinsic factors encompass external influences that contribute to reverse dental bone loss. These can arise from lifestyle choices, dental procedures, or traumatic events. Poor oral hygiene and certain dental treatments can inadvertently lead to bone resorption.
- Dental Procedures: Some dental procedures, such as extractions, implants, and extensive periodontal therapy, can inadvertently cause bone loss in the surrounding areas. The removal of teeth can trigger bone resorption in the adjacent areas. Surgical procedures can also impact the delicate balance of bone and tissue, potentially accelerating the process of bone loss.
- Trauma: Facial injuries or trauma to the jaw can lead to reverse dental bone loss. The impact can disrupt the delicate equilibrium of bone and tissue, potentially initiating bone resorption in the affected area.
- Inflammation: Chronic inflammation, often associated with gum disease (periodontitis), is a major culprit in reverse dental bone loss. The inflammatory response can disrupt the normal bone remodeling process, resulting in bone resorption.
- Oral Hygiene Habits: Poor oral hygiene practices, such as inadequate brushing and flossing, can lead to the accumulation of plaque and tartar. This buildup can result in inflammation and periodontal disease, contributing to reverse dental bone loss. A consistent and thorough oral hygiene routine is crucial for maintaining healthy gums and jawbones.
Risk Factor Comparison
| Risk Factor Category | Specific Factor | Mechanism | Prevention Strategies |
|---|---|---|---|
| Intrinsic | Genetics | Inherited predisposition to low bone density or metabolism. | Maintaining a healthy lifestyle, including a balanced diet and regular exercise, can help mitigate genetic predispositions. |
| Intrinsic | Age | Decreased bone turnover and natural physiological changes. | Adopting healthy habits early in life, including proper nutrition and regular exercise, can contribute to overall bone health. |
| Intrinsic | Systemic Diseases | Interference with bone remodeling processes. | Managing underlying systemic diseases with appropriate medical interventions and lifestyle modifications. |
| Extrinsic | Dental Procedures | Inadvertent bone resorption due to surgical or restorative interventions. | Minimizing invasive procedures when possible and ensuring meticulous post-operative care. |
| Extrinsic | Trauma | Disruption of the delicate equilibrium of bone and tissue. | Protective measures to minimize the risk of facial injuries and proper treatment of injuries. |
| Extrinsic | Inflammation | Disruption of normal bone remodeling processes. | Maintaining good oral hygiene practices, regular dental checkups, and addressing any signs of gum disease. |
| Extrinsic | Oral Hygiene Habits | Accumulation of plaque and tartar leading to inflammation. | Consistent and thorough oral hygiene routine, including brushing and flossing. |
Diagnosis and Assessment: Reverse Dental Bone Loss
Reverse dental bone loss, a disheartening condition affecting the supportive structures of teeth, requires meticulous diagnosis and assessment. Accurate identification is crucial for effective treatment planning and ultimately, preserving oral health. A comprehensive approach combines clinical evaluation with advanced imaging techniques to pinpoint the extent and cause of the bone loss.Understanding the nuances of reverse dental bone loss is critical to creating a personalized treatment strategy.
This involves not only identifying the presence of bone loss but also its precise location, severity, and potential underlying causes. A thorough diagnostic process, encompassing patient history, clinical examination, and advanced imaging, is essential to achieve this understanding.
Diagnostic Methods
Proper diagnosis of reverse dental bone loss necessitates a multifaceted approach. Clinical examination plays a fundamental role in evaluating the patient’s overall oral health and identifying potential signs of the condition. Patient history provides crucial context, revealing potential contributing factors like medications, lifestyle habits, and previous dental treatments.
Radiographic Techniques
Radiographic techniques are invaluable tools in detecting and evaluating the extent of reverse dental bone loss. These methods, including conventional radiographs and advanced imaging, offer detailed visualizations of the alveolar bone, crucial for assessing the degree of resorption. Precise identification of the bone loss’s location and severity allows for more targeted and effective treatment plans.
Imaging Modalities
Advanced imaging modalities like cone-beam computed tomography (CBCT) provide detailed three-dimensional (3D) images of the jawbone. These images allow for a comprehensive evaluation of the bone structure and the extent of the bone loss. The high resolution and detailed visualization enable clinicians to identify subtle changes in bone density and morphology that might be missed with conventional radiographs.
Clinical Assessments
Clinical assessments are critical for a comprehensive evaluation. These assessments involve a thorough examination of the teeth, gums, and supporting structures. This includes checking for mobility, inflammation, and any other signs of periodontal disease. This process, coupled with a detailed patient history, provides valuable information for a complete picture of the patient’s oral health status.
Bone Density Measurements
Bone density measurements are crucial in assessing the severity of reverse dental bone loss. These measurements, often incorporated into advanced imaging techniques, help quantify the amount of bone mineral density present. Lower bone density readings indicate a higher risk of further bone loss and increased susceptibility to future complications.
Cone-Beam Computed Tomography (CBCT)
Cone-beam computed tomography (CBCT) is a powerful imaging modality used to assess the extent of reverse dental bone loss. CBCT generates high-resolution 3D images of the jaw and teeth, providing a detailed view of the bone structure. This 3D visualization allows clinicians to precisely determine the location, extent, and severity of bone loss, which is essential for treatment planning.
Imagine a CBCT image of a patient with reverse dental bone loss. The image would show a clear visualization of the alveolar bone surrounding the teeth. The areas of reduced bone density would appear darker, highlighting the regions where bone loss has occurred. This detailed visualization allows for precise identification of the affected areas and quantification of the bone loss.
Diagnostic Tools
A table summarizing various diagnostic tools and their applications in evaluating reverse dental bone loss:
| Tool | Description | Advantages | Limitations |
|---|---|---|---|
| Conventional Radiographs | Two-dimensional X-rays of the teeth and jaw | Relatively inexpensive and readily available | Limited ability to visualize three-dimensional structures; may not detect subtle bone loss |
| Cone-Beam Computed Tomography (CBCT) | Three-dimensional X-rays of the jaw and teeth | Provides detailed 3D images, allowing for precise assessment of bone loss | More expensive than conventional radiographs; requires specialized equipment and expertise |
| Periodontium Examination | Clinical evaluation of gum tissues and teeth | Identifies signs of inflammation and bone loss | Subtle bone loss may be missed without additional imaging |
| Patient History | Gathering information about medical conditions, medications, and habits | Identifies potential contributing factors | Reliance on patient accuracy; potential for omissions or inaccuracies |
Treatment and Management Strategies
Reverse dental bone loss, a serious condition affecting the supporting structures of teeth, necessitates a multifaceted approach to treatment and management. Effective strategies aim to halt the progression of bone loss, restore lost structure, and maintain oral health. This often involves a combination of non-surgical and surgical interventions tailored to the individual patient’s needs and the severity of the condition.Addressing reverse dental bone loss requires a thorough understanding of the underlying causes and a commitment to a personalized treatment plan.
Successful management relies on early intervention, meticulous monitoring, and consistent patient cooperation. The goal is to prevent further bone loss, preserve existing teeth, and, where possible, restore a healthy, functional bite.
Non-Surgical Treatment Options
Non-surgical approaches are often the first line of defense in managing reverse dental bone loss. These methods focus on controlling the factors contributing to the bone loss and improving oral hygiene. A key component of non-surgical treatment is meticulous oral hygiene, including regular brushing, flossing, and professional cleanings. These practices help remove plaque and tartar buildup, which can exacerbate inflammation and bone loss.
- Periodontal Therapy: This encompasses a range of procedures aimed at controlling periodontal disease, the primary cause of many cases of reverse dental bone loss. Professional scaling and root planing are crucial in removing plaque and calculus from the tooth surfaces and root surfaces, smoothing them to prevent further bacterial colonization. Antibiotic therapy, in some cases, may also be employed to combat infection and inflammation.
- Lifestyle Modifications: Addressing potential contributing factors, such as smoking cessation, stress management, and a balanced diet rich in essential nutrients, can significantly impact the overall health of the gums and bone tissue. Patients with diabetes or other systemic conditions may require additional management strategies.
Surgical Treatment Options
Surgical interventions are often necessary when non-surgical approaches are insufficient to halt or reverse bone loss. The choice of surgical procedure depends on the extent and location of the bone loss, the patient’s overall health, and their specific needs.
Reverse dental bone loss can be a real head-scratcher, but luckily, there are ways to combat it. Thinking about how to best preserve the beauty of dried flowers, like those found in What to Do with Dried Flowers , can actually provide some inspiration. The meticulous care needed for dried botanicals mirrors the attention required to reverse bone loss, focusing on the delicate restoration of healthy oral structures.
- Bone Grafting: This involves replacing lost bone tissue with a suitable graft material. Various types of grafts are available, including autografts (from the patient’s own body), allografts (from a donor), and xenografts (from a different species). The specific type and method of bone grafting are chosen based on the individual patient’s circumstances. Techniques include guided bone regeneration (GBR), which uses membranes to encourage new bone formation in the area of bone loss.
- Guided Tissue Regeneration (GTR): This procedure uses a barrier membrane to prevent the ingrowth of unwanted connective tissue, allowing the bone to regenerate and repair lost structure. The specific type of membrane and surgical technique used are tailored to the particular site of bone loss.
Periodontal Therapy’s Role
Periodontal therapy plays a pivotal role in managing reverse dental bone loss. It focuses on controlling the underlying periodontal disease, which is a significant factor in bone loss. Treatment aims to reduce inflammation, eliminate infection, and promote the healing of damaged periodontal tissues. A comprehensive approach involves meticulous plaque control, professional cleanings, and, if necessary, antibiotic therapy.
Reverse dental bone loss is a tricky issue, impacting your overall oral health. It’s fascinating to see how different aspects of life can connect, like how someone’s post-band career path, as seen in a recent interview with Carlos D, a professional actor now giving a long interview about post-Interpol life here , can be indirectly linked to maintaining good oral hygiene habits to prevent such issues.
Ultimately, taking care of your teeth and gums is crucial for overall well-being, preventing this kind of bone loss.
Bone Grafting Methods
Bone grafting techniques for reverse dental bone loss vary depending on the specific needs of the patient. The procedures aim to provide a scaffold for new bone growth, restoring the lost supporting structure.
- Types of Grafts: Autografts, allografts, and xenografts each have unique characteristics and applications. Autografts offer the best biological match, but harvesting them can sometimes present surgical challenges. Allografts provide a readily available source of bone tissue, while xenografts offer a cost-effective alternative. The choice of graft material is often based on factors like cost, availability, and the specific characteristics of the defect.
Reverse dental bone loss is a real concern, and it’s often a complex issue. While the exact causes can vary, understanding the interplay of factors like oral hygiene and diet is crucial. Recent research into the potential benefits of la luz big big blood in supporting overall health, particularly related to blood circulation, might offer intriguing avenues for future study into preventing this bone loss.
Further investigation is needed to explore this connection and determine its effectiveness in reversing bone loss in the mouth.
- Techniques: Various surgical techniques, including guided bone regeneration (GBR) and guided tissue regeneration (GTR), are used in conjunction with bone grafting. GBR employs membranes to direct the growth of new bone tissue, while GTR focuses on preventing the unwanted ingrowth of connective tissue. Surgical precision is paramount in ensuring optimal outcomes and minimizing potential complications.
| Treatment Type | Description | Advantages | Potential Complications |
|---|---|---|---|
| Periodontal Therapy | Scaling and root planing, antibiotics, and lifestyle modifications | Non-invasive, cost-effective, often effective for early or mild cases | May not be sufficient for severe bone loss, requires patient compliance |
| Bone Grafting | Replacing lost bone with autografts, allografts, or xenografts | Potentially restores lost bone structure, promotes new bone growth | Risk of infection, graft rejection, limited success rates in certain cases |
| Guided Bone Regeneration (GBR) | Using membranes to direct new bone growth | Encourages bone regeneration, enhances success rates | Potential for membrane exposure, infection, and complications related to membrane placement |
| Guided Tissue Regeneration (GTR) | Using membranes to prevent unwanted tissue growth | Allows for controlled regeneration, improves outcomes | Potential for membrane exposure, infection, and complications related to membrane placement |
Prevention and Prognosis

Reverse dental bone loss, while often a challenging condition, is not always inevitable. Understanding the factors that contribute to its development, and more importantly, the proactive steps to mitigate its progression, is crucial for maintaining healthy smiles and overall oral health. This section will Artikel the preventive measures and discuss the prognosis based on severity, treatment, and patient adherence.Effective prevention relies on a multifaceted approach that combines meticulous oral hygiene, strategic dietary choices, and consistent dental care.
A proactive approach can significantly reduce the risk of bone loss and improve long-term oral health.
Preventive Measures to Minimize Risk
Maintaining optimal oral hygiene is paramount in preventing reverse dental bone loss. Regular brushing and flossing remove plaque and food particles that contribute to gum disease, a primary factor in bone resorption. Consistent professional dental cleanings are also essential for removing hard-to-reach plaque and tartar buildup. These preventive measures, when combined with a healthy diet and lifestyle, contribute to a significantly reduced risk of reverse dental bone loss.
Importance of Oral Hygiene and Regular Check-ups
Regular dental check-ups are crucial for early detection of gum disease and other oral health issues. Early intervention can halt the progression of bone loss and significantly improve the chances of successful treatment. Professional cleanings, performed every six months, remove accumulated plaque and tartar, preventing inflammation and reducing the risk of bone resorption. A dentist can identify any early signs of gum disease, such as bleeding gums or receding gums, which may indicate the beginning of bone loss.
Early diagnosis and intervention are key to preventing more severe complications.
Role of Dietary Factors and Lifestyle Choices
A balanced diet rich in essential nutrients supports overall health, including oral health. Vitamins, minerals, and antioxidants contribute to the maintenance of healthy gums and bone tissue. Smoking and excessive alcohol consumption significantly increase the risk of periodontal disease and subsequent bone loss. Maintaining a healthy weight, managing stress effectively, and getting adequate sleep are also crucial components of a comprehensive preventative approach.
Long-Term Consequences of Untreated Reverse Dental Bone Loss
Untreated reverse dental bone loss can lead to a cascade of adverse effects. Significant bone loss can compromise the stability of teeth, making them susceptible to shifting, loosening, and eventual loss. Advanced gum disease, if left untreated, can also lead to significant pain, discomfort, and an overall diminished quality of life. The aesthetic impact of bone loss can be substantial, leading to a noticeable change in the shape and appearance of the smile.
Prognosis of Reverse Dental Bone Loss
The prognosis for reverse dental bone loss depends heavily on the severity of the condition, the treatment received, and the patient’s commitment to following the prescribed treatment plan. Early intervention and diligent adherence to a prescribed treatment plan significantly improve the chances of successfully halting or reversing bone loss. The prognosis for mild cases is often favorable, with appropriate treatment, and consistent oral hygiene practices, preventing further bone loss.
However, advanced cases, particularly those with extensive bone loss, may require more complex treatments, potentially leading to less predictable outcomes. Factors such as patient compliance, lifestyle choices, and overall health play significant roles in determining the ultimate outcome.
Final Thoughts
In conclusion, reverse dental bone loss is a multifaceted issue demanding a nuanced approach. The intricate interplay of intrinsic and extrinsic factors, combined with the critical role of proper diagnosis and personalized treatment plans, makes understanding this condition essential. Ultimately, by understanding the full scope of this issue, patients and professionals can work together to improve outcomes and maintain optimal oral health.